
Lumbar Disc Injury
Slipped disc? Bulging Disc? What you need to know.
Following on from our Acute Lower Back Pain blog a few weeks ago (have a read of that here), we are going to discuss spinal disc injuries. We will go a little deeper into the dreaded ‘bulging disc’ and how it can be managed. As discussed in our previous post, back pain can be divided into 2 categories; Specific and Non specific.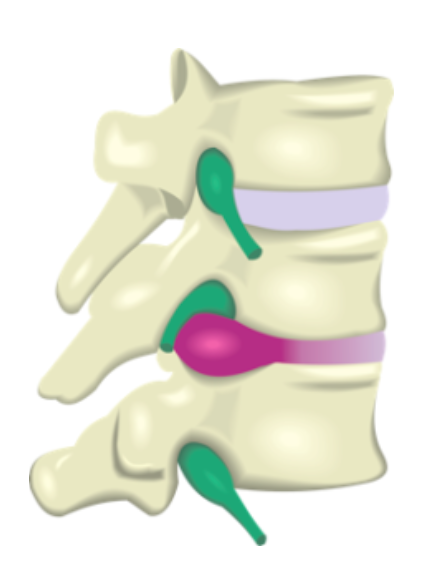
- Non specific back pain – is not caused by any specific pathology. It is usually as a result of joint or muscle strain and is often due to mechanical problems. This is the majority of what we see in practice with over 90% of low back pain considered to fall into this category. This is well managed with manual therapy, specific exercises and activity/posture modification.
- Specific back pain – is less common and is caused by more serious conditions such as fracture, arthritis, scoliosis, nerve impingement, growths, disc problems or infections.
When we break Specific low back pain down, we see that less than 1% of people have pain due to fracture, growths/tumour, infection or due to an inflammatory process. About 5% of people have nerve irritation/inflammation which results in a loss of sensory and motor control in the legs.
THE DISC
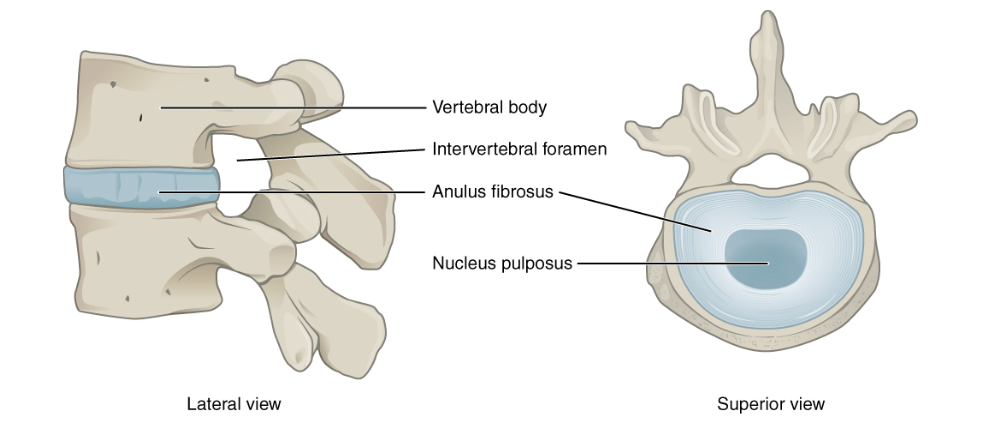
In between every one of the little vertebral bones in your back you have an intervertebral disc (IVD). The IVD’s are strong elastic structures made up of 2 components; the annulus fibrosis on the outside and a gel like structure on the inside, known as the nucleus pulposus. When a disc is injured through a tear or age related changes, sometimes the nucleus pulposus is able to move through the external portion (where the ‘bulging’ term comes from) of the IVD and if large enough can irritate surrounding nerves and structures.
Despite popular belief, it is often NOT one incident but a cascade of micro trauma and weakening over a long period of time that causes IVD injuries.
If the irritation to the nerve is enough, you may experience ‘Radiculopathy’. This is when the disc is irritating the nerves in the area, Resulting in numbness, tingling or pain down the lower back, glutes/hip and legs. While they can be extremely painful early, the good news is the majority of these disc injuries resolve within 3-6 months. While most patients will have improvement within 4-6 weeks. Surgery is very rarely needed unless you progressively lose muscle power.
Now, it is important to remember that just because you have a ‘disc bulge’ on an MRI scan doesn’t mean you will have pain. 80% of people without back pain have age related degenerative changes to the IVD’s and 50% of people without pain have ‘bulges’.
OSTEO AND DISC INJURIES
- We will be about to chat about some small modifications you can make to your daily routine to avoid aggravating the symptoms
- Your osteopath will perform a complete assessment and determine a diagnosis of your pain.
- Osteopathic techniques to the surrounding muscles and joints; including soft tissues, dry needling. joint articulation, muscle stretching and mobilization can be used to help reduce tension and inflammation.
- Gentle and appropriate exercise to your ability and pain tolerance
- Recent research suggests that keeping active and moving the lower back rather then bed rest will help decrease pain and improve function faster. Bed rest also associated with other complications such as depression and anxiety
References:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4761624/
- Long, Suzanne & E Surrey, David & Nazarian, Levon. (2013). Sonography of Greater Trochanteric Pain Syndrome and the Rarity of Primary Bursitis. AJR. American journal of roentgenology. 201. 1083-6. 10.2214/AJR.12.10038
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5294943/
- https://www.nps.org.au/australian-prescriber/articles/managing-low-back-pain-in-primary-care
- Brinjikji W, Luetmer PH, Comstock B, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2014;36(4):811–816. doi:10.3174/ajnr.A4173
