Is watching the tennis reminding you about the sore elbow that is still bothering you?
As discussed in our last blog you don’t need to play tennis to suffer from “tennis elbow”.
If you have tennis elbow, one of the most effective ways to help manage it is through strengthening exercises. Here is a simple one you can do at home to start with:
– Start in a seated position with your affected elbow and wrist resting on a table, palm facing down
– Place your opposite hand over the hand on your affected side
– Try to push the hand on your affected side up towards the ceiling, while resisting the movement with your opposite hand (so the muscles in your forearm contract but no movement occurs at your wrist or elbow)
– Hold for 10 seconds
This exercise should not cause any pain so if you do experience pain in your elbow while doing this exercise, please stop.
Elbow pain can be debilitating and can come from various causes. If you are suffering from elbow pain and are not sure what’s causing it, make a booking with one of our osteopaths for a complete assessment and we will help to advise you on the types of treatment and management appropriate for your condition.

Feeling the tension in your neck and shoulders? Do you suffer from upper back pain?
Decreased mobility through the ribs and thoracic spine can cause tightness and stiffness in the upper back, chest and neck. Here is a simple exercise you can do at home to help improve mobility and reduce tension through these areas:
– Lie on your side with your head supported on a pillow and your knees bent between 90 and 120 degrees.
– Reach your arms out in front of you, with your hands together.
– Rotate the upper arm upwards and outwards (in a windmill type action).
– Try to rotate as far as you can, without any pain through the shoulder and ribs.
– Take 2 breathes and return to starting position. Repeat 10-15 each side in the morning.
– For an extra stretch, you can drop your top knee off your bottom knee and closer to the floor.
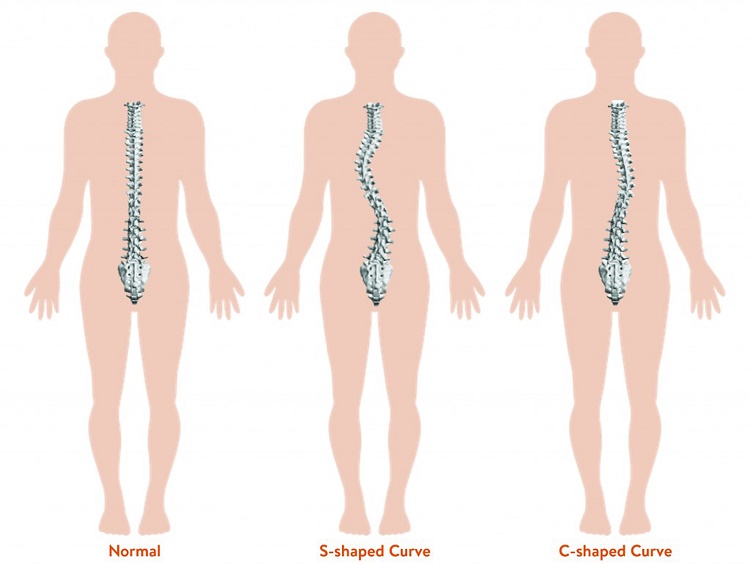
The spine is made up of vertebrae that stack up one on top of the other separated by discs. Looking from behind the spine usually stacks up with one vertebrae straight on top of the one beneath. In scoliosis however the spine is deviated from the midline creating a ‘C’ or ‘S’ shape curve. This deviation from the midline is a combination of the vertebrae curving to the side coupled with rotation.
Scoliosis can vary from a mild curve causing little or no symptoms to a severe curve, which may require treatment. Treatment is most effective when the scoliosis is detected early and managed with appropriate strategies based on the degree of curve.
There are several different types of scoliosis
- Congenital
- Neuromuscular
- Idiopathic – this is the most common form and is classified according to when onset was identified – infantile, juvenile, adolescent or adult. The most common type is adolescent idiopathic scoliosis (AIS). We will further discuss AIS in this blog.
Adolescent Idiopathic Scoliosis (AIS)
- Girls are affected 8-10 times more than boys
- Only 3 in 1000 girls will require further treatment
- There is often no pain or other symptoms at the time of diagnosis
- The exact cause of AIS remains unknown but it is important to note it is NOT caused by “bad posture”, a soft mattress, watching too much TV or carrying a heavy school bag, although these things may exacerbate symptoms.
- The most significant risk factor for developing AIS is a family history of the condition.
It is important to screen for AIS at key ages. The Spine Society of Australia recommends screening at 10 and 12 years of age as this is the usual age for the largest growth spurt and the first signs of scoliosis.
A fact sheet is routinely distributed to girls in school with information for home screening. You can find this fact sheet here.
Signs of Scoliosis
- Uneven shoulder heights
- Uneven shoulder blades or one shoulder blade that seems more prominent
- Uneven hips or one hip that seems more prominent
- More of a gap between the arm and waist on one side
- An obvious curve in the spine
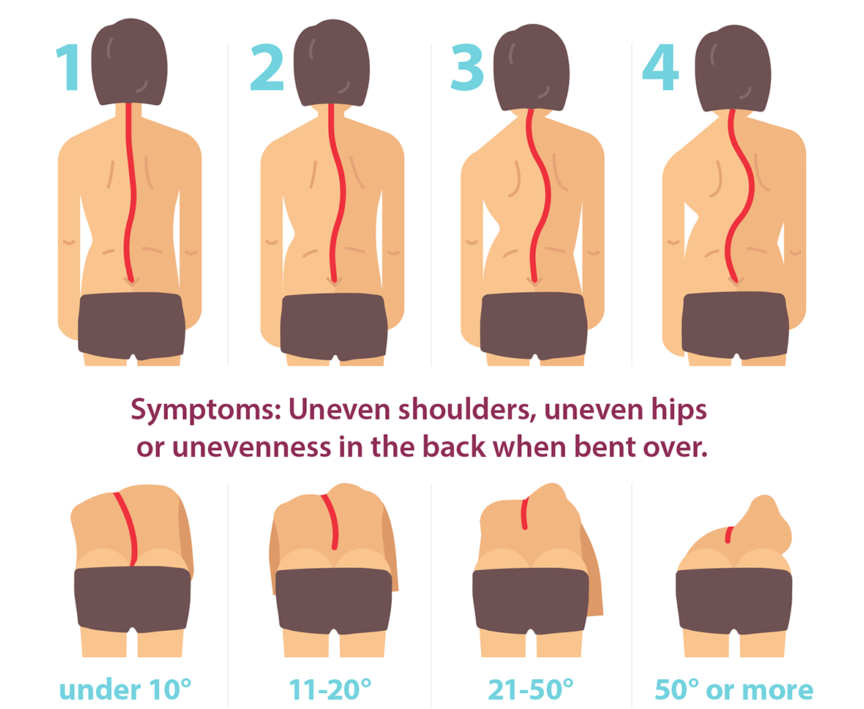
Image supplied by National Scoliosis Centre
The curve of the scoliosis can be classified according to how mobile it is:
Structural scoliosis is a fixed curve in the spine and the most common form in Adolescent Idiopathic Scoliosis (AIS). A structural curve usually has a physical structural change in the vertebrae.
Functional scoliosis is not structurally fixed. That is, the curve will bend with movement and may straighten again. It can be caused by:
– muscle spasm as a result of injury or compensation for a structural scoliosis curve
– overuse of the muscles on one side of the spine due to sport or occupation
– a difference in leg lengths
A note on scoliosis in adults:
– scoliosis may be first diagnosed in adulthood if a previously undiagnosed AIS curve has progressed.
– scoliosis may also develop in adulthood secondary to degenerative changes in the spine such as osteoarthritis and degenerative disc disease.
How Osteopathy can assist
Treatment for scoliosis varies depending on the type and severity of the curve.
Our osteopaths will perform a complete assessment, including specific scoliosis screening tests, determine a diagnosis of your pain and refer you if an x-ray or specialist assessment is required.
Osteopathic techniques including joint articulation/mobilisation and soft tissue release may help to improve spinal mobility, reduce back muscle tension and decrease pain.
Exercise, strengthening and stretching are important parts of maintaining spine health and our osteopaths can chat to you about some options and tailor a program to you.
If we assess the scoliosis to be severe and requiring different treatment such as bracing, our Osteopaths can refer you to the appropriate health professionals.
If you would like your spine assessed or your child’s screened for Scoliosis, contact us or make a booking here
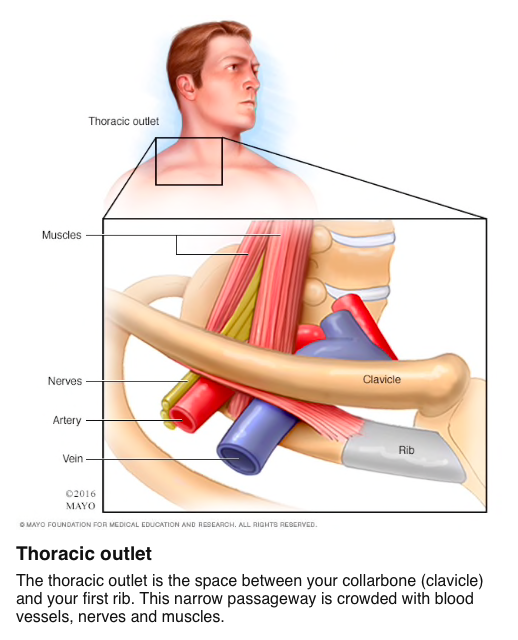
Are you experiencing pain, altered sensation or heaviness in your arm? It could be thoracic outlet syndrome.
Thoracic outlet syndromes (TOS) are a group of conditions that occur when there is compression or irritation to the nerves or blood vessels as they pass through the ‘thoracic outlet’, or as they travel from your neck towards your armpit. The brachial plexus, which is the bundle of nerves that supply the upper body and the subclavian vessels (vein and artery) run through the outlet. It is more common in women, and people 20-50 years old.
Signs and Symptoms
Thoracic outlet syndrome can present with symptoms of either nerve or blood vessel compression, or a combination of both. Nerve compression is the most common and usually presents with pain, altered sensation, weakness, and occasionally loss of muscle tone in the arm. The venous type results in swelling, pain, and change of circulation leading to sweating, blue tinged discoloured skin and blotchiness of the arm. The arterial type results in pain, coldness, and paleness of the arm. These might be happening individually or together.
What causes Thoracic Outlet Syndrome?
- Compression of nerves or arteries due to tight muscles
- Injury to the artery due to bony abnormality
- Injury or compression of the vein.
- Trauma
- Repetitive arm movements causing hypertonic neck and chest muscles
- A congenital abnormality
- Tumour
- Pregnancy
How can osteopathy help?
- Our osteopaths will complete a full assessment, diagnosis and management plan for your symptoms
- We have specific tests we can use to determine if it is thoracic outlet syndrome or other conditions causing your symptoms.
- We can use techniques like soft tissues, joint mobilization and stretching to help reduce muscle tension around the thoracic outlet
- These techniques may help promote blood flow and lymphatic drainage to help reduce inflammation and swelling
- Advise on some daily modifications you can make to help reduce symptoms.
- Prescribe some basic exercises to help with abdominal breathing, posture correction and postural strengthening, all important components of recovering from thoracic outlet syndrome.
If you would like to discuss this further with one of our Osteopaths book in online here.
References:
- Jones et al., (2019). Thoracic outlet syndrome: A comprehensive review of pathophysiology, diagnosis and treatment.
Do you have stiffness in your shoulder that has started for no apparent reason? Do you have severe pain in your shoulder, which is particularly painful at night? Are you finding it difficult to move your arm and reach as far as you used to be able to? This could be a frozen shoulder.
What is frozen shoulder?
Frozen shoulder is a common term used to describe the condition “adhesive capsulitis”, which involves a thickening and contracture of the capsule and connective tissues surrounding the shoulder joint.
The common three phases of a frozen shoulder are:
“Freezing” (becoming painful)
– Pain becomes increasingly severe, often worse at night
– Shoulder begins to become stiff, often first losing the ability to fully reach overhead or rotate the arm backwards.
– This period typically lasts 2-9 months
“Frozen” (stiffness)
– Pain is less severe
– There is considerable shoulder stiffness, affecting activities of daily life
– This period typically lasts 4-12 months
“Thawing” (resolving)
– Pain resolves
– Shoulder range of motion is gradually restored
– This period typically lasts 5-26 months
What causes it?
It is still unknown what exactly causes frozen shoulder.
It can sometimes start after a shoulder injury or surgery but more often there is no underlying cause. Some conditions such as diabetes and connective tissue disorders may increase the likelihood of developing frozen shoulder.
It most commonly occurs in the 40-60 year old age group and is more likely to affect women than men.
Osteopathy and Frozen Shoulder
In the early stages of frozen shoulder it can be difficult to differentiate the symptoms from a number of other shoulder conditions so our osteopaths will perform a careful assessment to determine a diagnosis of your pain.
Each phase of frozen shoulder requires a different approach and form of treatment so our osteopaths will tailor a treatment and management plan to suit you. The symptoms of frozen shoulder can be flared up by inappropriate treatment and management so it is important to seek advice early on.
Our Approach
- Osteopathic techniques including soft tissue massage, joint articulation, muscle stretching and mobilisation may be used to help relieve pain and reduce muscle tension around the shoulder.
- A program of appropriate gentle stretching and strengthening exercises may help to improve shoulder movement and maintain muscle strength.
- Our osteopaths will also chat to you about some small modifications you can make to your daily routine to avoid aggravating the symptoms.
References
Itoi E et al: Shoulder stiffness: current concepts and concerns. Arthroscopy. 32(7):1402-14, 2016
Le HV et al: Adhesive capsulitis of the shoulder: review of pathophysiology and current clinical treatments. Shoulder Elbow. 9(2):75-84, 2017
Georgiannos D et al: Adhesive capsulitis of the shoulder: is there consensus regarding the treatment? A comprehensive review. Open Orthop J. 11:65-76, 2017
Hsu JE et al: Current review of adhesive capsulitis. J Shoulder Elbow Surg. 20(3):502-14, 2011
Ewald A: Adhesive capsulitis: a review. Am Fam Physician. 83(4):417-22, 2011
Page MJ et al: Manual therapy and exercise for adhesive capsulitis (frozen shoulder). Cochrane Database Syst Rev. CD011275, 2014
Learn more about what can be causing your shoulder pain and how our Osteopaths can help
The rotator cuff is a group of 4 muscles that are responsible for…rotating the shoulder. They are also very important in shoulder stabilization, by helping depress the shoulder to allow for greater movement. Given the large amount of movement allowed through the shoulder joint it is not uncommon for people to develop pain in this area.
Rotator cuff injuries/weakness are a significant cause of shoulder pain. They occur mainly in patients between 40 and 60 years of age and may be from trauma, but many do not involve an injury. They can slowly evolve from deconditioning, weakness and or overuse.
Patients might find that the pain can move around their shoulder. Given the close proximity of all the structures, they may experience pain at the front, back or side of the shoulder. Actions like hanging out the washing or movements like putting on a jacket may flare it up.
Below we will discuss some different types of rotator cuff pain but first a very brief shoulder anatomy lesson – The shoulder is made up of 3 bones – the humerus (upper arm bone), clavicle (collar bone) and the scapula (shoulder blade). These 3 bones makes a ‘little tunnel’ for all the rotator cuff tendons to run through and they attach directly onto the Humerus bone. To help reduce friction and absorb some shock in this space there is a little sac of fluid called a bursa.
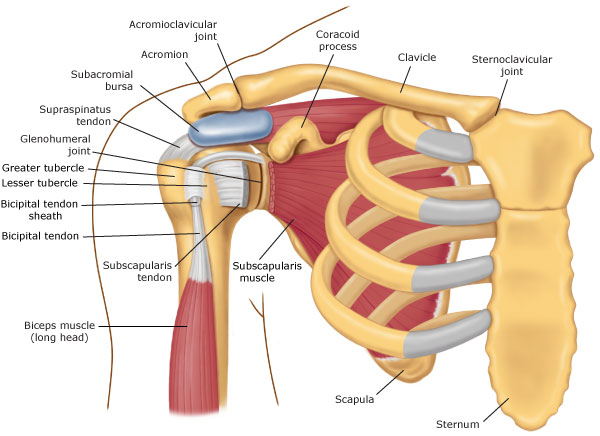
Types of Rotator Cuff injuries:
Shoulder Impingement or Shoulder Tip Pain: When you lift you arm above your head, the space where the rotator cuff tendons run narrows, this can lead to compression of the tenson and can cause pain and irritation.
Bursitis: Just like the tendons, this can become irritated. Inflammatory cells infiltrate the sac and can become a shoulder irritant, ‘generally’ bursitis is a secondary finding to another issues in the shoulder
Rotator cuff tears: Rotator cuff tears can occur in people from direct trauma, like a fall or accident (less likely) or due to repetitive actions over time (more likely). A study has recently found that 54% of asymptomatic (i.e. not having pain or problems) patients aged 60 years or over, were found to have partial or complete tears of the rotator cuff on MRI. This shows us that tissue damage doesn’t always equal pain.
Tendinopathies: This is a general term used to describe cellular changes to the tendons of the rotator cuff over time, due to overload.
OSTEOPATHY AND SHOULDER PAIN
- Our osteopaths will perform a complete assessment and determine a diagnosis of your pain.
- Osteopathic techniques including soft tissues, joint articulation, muscle stretching and mobilization may be used to help reduce muscle tension of the shoulder, thoracic spine, neck and arm.
- May help promote blood and lymphatic flow, helping reduce pain and inflammation.
- Education re exercise program/modification
- Chat about some small modifications you can make to your daily routine to avoid aggravating the symptoms
Book an appointment to chat with one of our osteopaths about your shoulder pain HERE
DEALING WITH ELBOW PAIN? READ ON TO FIND OUT HOW WE CAN HELP.
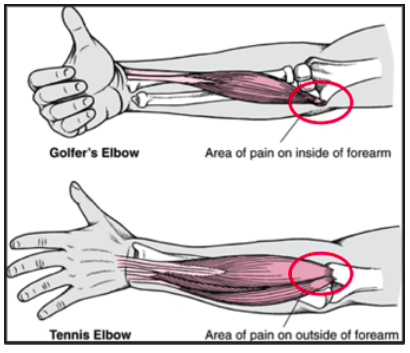
Have you heard of Golfer or Tennis elbow? Do you have elbow pain but don’t play either? Elbow pain can be extremely painful and debilitating, the 2 most common musculoskeletal conditions to affect the elbow are commonly referred to as ‘Tennis elbow’ and ‘Golfer’s elbow’ however the majority of our patients who present with elbow pain surprisingly don’t play either.
Tennis elbow, or lateral elbow tendinopathy affects the tendons on the outside of the elbow and is caused by overuse & repetitive loading of the wrist extensor muscles (on their attachment sites to the elbow). Golfer’s elbow or medial elbow tendinopathy and is caused by overuse & repetitive loading of the wrist flexor muscles. Golfer’s elbow is much less common than Tennis elbow, with Golfer’s elbow only 9-20% off all tendinopathies of the elbow.
We know that tendon pain (tendinopathy) is not due to inflammation but rather degeneration and disorganization of the tendon usually due to a change in load…ie more gardening, computer work, or home duties, you don’t have to play the sports or lift super heavy weights. Small changes in load repetitively can create the same issue.
Risk factors
It most commonly presents in men and women between the ages of 35-60
Smoking and other systemic factors such as obesity and diabetes.
Manual workers (repetitive movements of the wrist)
Tennis players (40% will be affected at some point in their ‘career’)
Sports such as golf, baseball, weight lifting and rowing,
Signs and symptoms:
Decrease function of the elbow and surrounding muscles
Tenderness over the outside of the elbow (tennis) or inside (golfers)
Pain on gripping or general everyday things, ie opening jars and mouse/computer work
Tennis elbow – Pain on wrist extension (action of acceleration on motor bike, the wrist is slightly extended on typing on your keyboard )
Golfers elbow – pain on wrist flexion (opposite of above)
Osteopathy and Elbow pain
Our osteopaths will perform a complete assessment and determine a diagnosis of your pain. While the diagnosis of elbow pain is generally straightforward, management needs to be tailored to each patient.
Osteopathic techniques including soft tissues, joint articulation, muscle stretching and mobilization may be used to help reduce muscle tension of the elbow, wrist and forearm
Chat about some small modifications you can make to your daily routine to avoid aggravating the symptoms
Tendinopathy’s DO NOT IMPROVE WITH REST.
To decrease tendon pain, you need to modify the load going through the area.
Exercise has the most evidence for treatment of tendon pain. These tendons are angry, we need to use them correctly. A tailored exercise plan will slowly help the tendon regenerate and repair.
Tends generally respond slowly to treatment and it can be very frustrating.. Patience is important, exercises should be correct and progressed appropriately.
References:
– https://www.jospt.org/doi/full/10.2519/jospt.2015.5841
-https://www.raynersmale.com/blog/2017/2/10/lateral-epicondylalgia-pathophysiology-assessment
– https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4990766/
– Amin NH, Kumar NS, Schickendantz MS. Medial epicondylitis: evaluation and management. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2015 Jun 1;23(6):348-55.
Slipped disc? Bulging Disc? What you need to know.
Following on from our Acute Lower Back Pain blog a few weeks ago (have a read of that here), we are going to discuss spinal disc injuries. We will go a little deeper into the dreaded ‘bulging disc’ and how it can be managed. As discussed in our previous post, back pain can be divided into 2 categories; Specific and Non specific.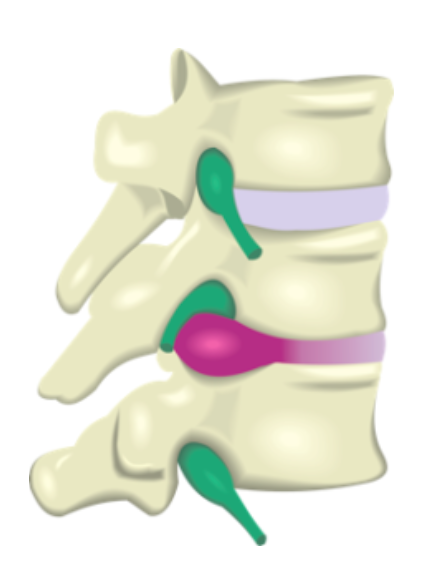
- Non specific back pain – is not caused by any specific pathology. It is usually as a result of joint or muscle strain and is often due to mechanical problems. This is the majority of what we see in practice with over 90% of low back pain considered to fall into this category. This is well managed with manual therapy, specific exercises and activity/posture modification.
- Specific back pain – is less common and is caused by more serious conditions such as fracture, arthritis, scoliosis, nerve impingement, growths, disc problems or infections.
When we break Specific low back pain down, we see that less than 1% of people have pain due to fracture, growths/tumour, infection or due to an inflammatory process. About 5% of people have nerve irritation/inflammation which results in a loss of sensory and motor control in the legs.
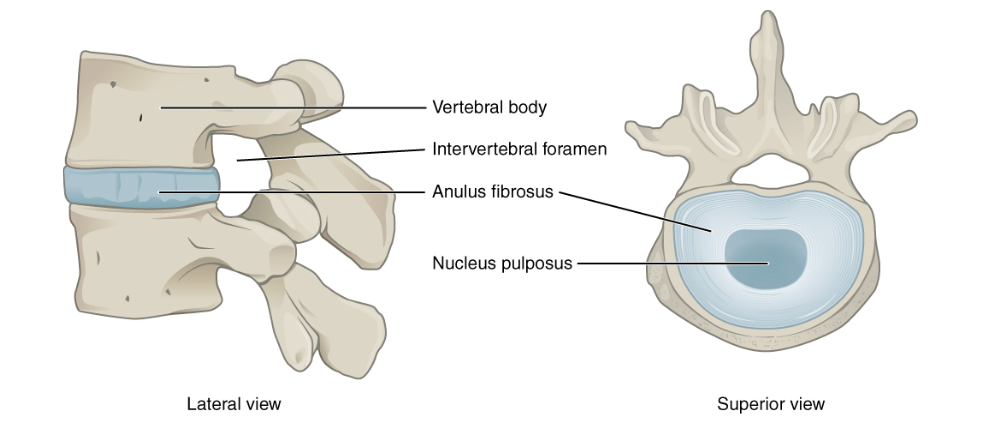
THE DISC
In between every one of the little vertebral bones in your back you have an intervertebral disc (IVD). The IVD’s are strong elastic structures made up of 2 components; the annulus fibrosis on the outside and a gel like structure on the inside, known as the nucleus pulposus. When a disc is injured through a tear or age related changes, sometimes the nucleus pulposus is able to move through the external portion (where the ‘bulging’ term comes from) of the IVD and if large enough can irritate surrounding nerves and structures.
Despite popular belief, it is often NOT one incident but a cascade of micro trauma and weakening over a long period of time that causes IVD injuries.
If the irritation to the nerve is enough, you may experience ‘Radiculopathy’. This is when the disc is irritating the nerves in the area, Resulting in numbness, tingling or pain down the lower back, glutes/hip and legs. While they can be extremely painful early, the good news is the majority of these disc injuries resolve within 3-6 months. While most patients will have improvement within 4-6 weeks. Surgery is very rarely needed unless you progressively lose muscle power.
Now, it is important to remember that just because you have a ‘disc bulge’ on an MRI scan doesn’t mean you will have pain. 80% of people without back pain have age related degenerative changes to the IVD’s and 50% of people without pain have ‘bulges’.
OSTEO AND DISC INJURIES
- We will be about to chat about some small modifications you can make to your daily routine to avoid aggravating the symptoms
- Your osteopath will perform a complete assessment and determine a diagnosis of your pain.
- Osteopathic techniques to the surrounding muscles and joints; including soft tissues, dry needling. joint articulation, muscle stretching and mobilization can be used to help reduce tension and inflammation.
- Gentle and appropriate exercise to your ability and pain tolerance
- Recent research suggests that keeping active and moving the lower back rather then bed rest will help decrease pain and improve function faster. Bed rest also associated with other complications such as depression and anxiety
References:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4761624/
- Long, Suzanne & E Surrey, David & Nazarian, Levon. (2013). Sonography of Greater Trochanteric Pain Syndrome and the Rarity of Primary Bursitis. AJR. American journal of roentgenology. 201. 1083-6. 10.2214/AJR.12.10038
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5294943/
- https://www.nps.org.au/australian-prescriber/articles/managing-low-back-pain-in-primary-care
- Brinjikji W, Luetmer PH, Comstock B, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2014;36(4):811–816. doi:10.3174/ajnr.A4173
If you are struggling with pain on the side of the hip, our Osteopaths we can assist you using evidence based rehabilitation and education along with hands on manual therapy.
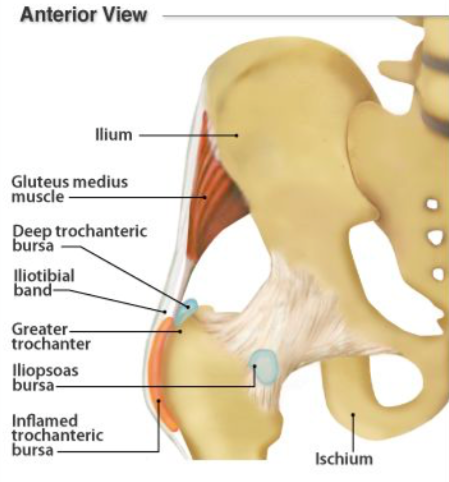
Greater trochanteric pain syndrome (GTPS) is new general term used to describe pain on the lateral hip. The greater trochanter is the bony prominence on the lateral side of the leg bone, near the hip. If you are struggling with pain in this area we can assist you using evidence based rehabilitation and education along with hands on manual therapy.
GTPS is a combination of gluteal tendinopathy and bursal irritation. Research has shown us that bursal irritation is almost always a secondary finding due to a gluteus minimus or medius tendon issue.
The likely cause of GTPS is by repetitive friction between the greater trochanter and Iliotibial band (ITB), this causes ongoing compression/microtrauma to the gluteal tendons where they insert onto the greater trochanter. This can develop into gluteal tendinopathy – degeneration and disorganization of the area. This leads to weakened gluteal muscles, de-stabilizing the hip and creating local pain and inflammation (bursal irritation).
Symptoms of GTPS:
- Pain over the greater trochanter/lateral hip
- Pain that radiates down the outside of the leg to the knee or into the buttock
- Pain when sleeping on the affected side, walking up hills or stairs.
- You may struggle to stand on one leg, ie to put pants on.
Risk factors:
- All ages groups, however women, 40-60 years old are commonly affected
- Recent change in load; tendons can struggle with this
- Use of corticosteroids
- Genetics
Osteopathy and GTPS
- Your osteopath will perform a complete assessment and determine a diagnosis of your pain.
- Take home modifications to your daily living are just as important as any hands on treatment. So we will chat through them with you…see below for some easy tips.
- We will perform manual therapy techniques such as soft tissue and joint release. This may help reduce muscle tension around the gluteal muscles, lower back, thigh, groin and knee to help decrease pain and improve range of movement.
- Techniques to help promote blood and lymphatic flow, helping reduce pain and inflammation.
- Our osteopaths will create a management plan, including strength base exercises to help reduce the compression through the lateral hip.
TAKE HOME TIPS
- So my ITB is tight, Should I foam roll it? Short answer, no. The ITB isn’t a muscle, it is the longest tendon in the body, so we can’t change the length of it. As we mentioned above, most of the pain experienced with GTPS is from compression. So we want to minimise any compression and direct pressure on the area including repeated pressure from a foam roller.
- So what do we do? The tensor fasciae latae (TFL) is a small muscle on the side of the hip that runs directly into the ITB. It along with the gluteal muscles play are large part in the the tension of the ITB. Releasing these muscles may have a great effect on the ITB.
- Sleeping tips: Avoid laying directly on that side, sleep with a pillow in between your knees.
- Sitting and standing tips: Avoid sitting with your legs crossed, leaning on one leg while standing and over stretching your glute muscles
References:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4761624/
- Long, Suzanne & E Surrey, David & Nazarian, Levon. (2013). Sonography of Greater Trochanteric Pain Syndrome and the Rarity of Primary Bursitis. AJR. American journal of roentgenology. 201. 1083-6. 10.2214/AJR.12.10038
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5294943/
Pregnancy is one of the most significant times of physical change in a woman’s body throughout her life. These changes happen in a relatively short period of time often resulting in extra stress on the muscles and joints.
Health and Balance osteopathy will support you through your pregnancy by providing gentle and safe treatment. This will help your body to adapt to the demands and physical changes during this time. We will also guide you on appropriate exercises or specific stretching to compliment the treatment we are providing. Contact us today to arrange an appointment.
Why visit an osteopath when pregnant?
Osteopathy provides many benefits for pregnant women. Some of the reasons a woman may consult an osteopath during her pregnancy include:
– ensure their body adjusts well to the physical changes of pregnancy
– reduce the effects of extra strain, weight and pressure on the joints of the spine and lower limb
– relief from lower back pain, middle back pain, upper back pain and neck pain
– relief from sciatica
– reduce effects of swelling that can often result in carpal tunnel syndrome
– manage pelvic instability and pelvic girdle pain
– closer to labour ensuring optimal foetal position to assist in ease of labour
Reducing the physical strain on the body allows precious energy to go into growing a healthy bub and enjoying a comfortable pregnancy.
Contact our Melbourne team for osteopathy pregnancy services
If you’re interested in osteopathy while pregnant, please get in touch with our experienced team by calling us directly on (03) 9999 8075 or by emailing tammy@healthandbalance.com.au and we’ll get back to you as soon as possible. Alternatively, you can book your appointment via our online booking system.
We work closely with your prenatal health professionals providing a consistent team care arrangement having good relationships with midwifes and obstetricians of Mercy hospital in Heidelberg along with other leading maternity hospitals in Melbourne.









